What CTOs Overlook in RPM: Data Routing, Alerts, and Escalation Logic
Remote Patient Monitoring is transforming chronic care, post-discharge follow-up, and preventative healthcare. However, although many healthcare CTOs and product teams prioritize device integration and patient onboarding, essential system design areas, such as RPM data routing, clinical alerts, and escalation processes, are sometimes overlooked.
For CTOs in charge of RPM infrastructure at healthcare providers, digital health startups, or SaaS platforms, omitting these components might result in significant alert fatigue, data overload, and slow responses. In this blog, we’ll examine what’s often overlooked and how technical leaders can adapt to create scalable, intelligent RPM systems that enable faster and more effective care choices.
RPM Data Routing
Most RPM platforms gather patient vitals such as blood pressure, glucose, weight, and oxygen saturation, but what happens to the data afterwards? That is the essential, frequently neglected question.
Common Routing Mistakes
- Include one-way data dumps into EHRs without filtering or relevance mapping.
- Flat storage in data lakes with no downstream actionability.
- There is no prioritizing based on patient condition, treatment pathway, or provider function.
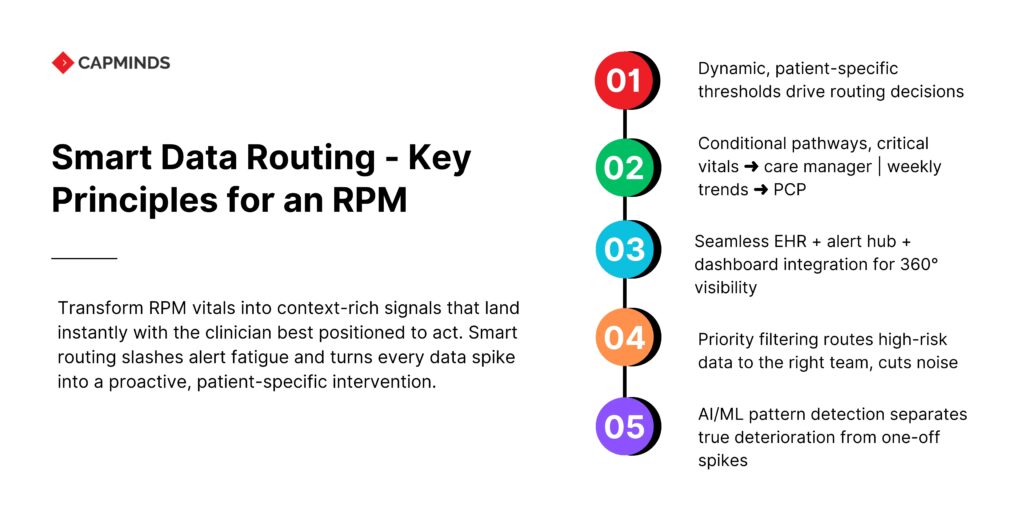
Smart Data Routing
To motivate action, RPM data should be routed contextually across your architecture.
- Dynamic routing is based on thresholds and patient-specific regulations.
- Conditional routing: For example, aberrant vitals are routed to a care manager, while trends are routed to the PCP weekly.
- EHR + Alert System + Clinical Dashboard Integration to improve situational awareness across care teams.
Best Practices
- Implement condition-specific routing logic to send diabetes data to endocrinology teams.
- Send high-priority vitals to nurse triage teams, not general inboxes.
- Use AI/ML models to identify worsening patterns vs isolated outliers.
Turning RPM Data into Rapid Decisions
Clinical notifications are intended to prompt immediate action. However, when notifications are overused or improperly structured, they cause alert fatigue, a hazardous condition in which providers overlook or disregard cautions, sometimes important ones.
Symptoms of poor alert design include:
- The same alert is being sent numerous times each day for minor variations.
- Alerts are based on static thresholds, not customizable ranges.
- Notifications contain no context, such as trend, patient risk score.
CTOs should understand that using static thresholds, such as BP > 140/90, is ineffective in a population with diverse comorbidities and baseline conditions. RPM systems require contextualized alert logic that is tailored to each patient.
Escalation Protocols
Even if the correct warning is delivered to the appropriate doctor, what happens next? Alerts may be delayed if there is no clear escalation logic. This gap converts RPM into a passive system rather than a responsive one.
Some common escalation failures include:
- Assigning an alert to an off-duty or overworked staff member.
- No reaction trigger, the alarm remains unresolved.
- There is no record of follow-up activities or results.
An effective escalation framework includes:
- Role-based escalation tree: RN -> NP -> Physician
- Time-based triggers escalate if not handled within 15 minutes.
- Audit trails record each alert, reaction, and resolution step.
A patient’s oxygen saturation falls below 88%. If the alarm is not handled within 10 minutes, it automatically escalates to the respiratory team and, if necessary, initiates a home care dispatch.
Real-Time Routing
In RPM design, CTOs must differentiate between:
- High-frequency vitals, such as heart rate from wearables,
- Daily summary readings from glucometer inputs.
- One-time survey replies, such as symptom check-ins.
- Each requires a unique routing path and urgency level.
Best Practices in Real-Time RPM Routing:
- Create real-time streams for high-risk patient segments such as post-surgical patients.
- To decrease noise, use batch processing with non-critical metrics.
- Use edge computing to filter out irrelevant data at the device level.
The Importance of Real-Time Processing in RPM Success
Healthcare does not wait, and neither should your RPM data. Real-time data routing enables providers to operate inside the golden window of intervention. However, not every data deserves equal urgency.
Categorize incoming RPM data into:
- Immediate Action, like heart rate abnormalities
- Daily Review, like blood glucose records
- Long-term trends in weight after 30 days
This reduces alert clutter and directs attention to the most important information. Technologies for Real-Time RPM include:
- FHIR subscriptions and push-based event alerts.
- MQTT and WebSockets provide lightweight, real-time communication.
- Edge computing: filtering unnecessary data at the device level.
Integration & Interoperability
Your RPM system is only as effective as it can connect with the rest of the health IT ecosystem. However, CTOs frequently postpone EHR and care coordination technology interfaces, resulting in separate data gaps. What You Need:
- FHIR-based data models for standardized exchange.
- API orchestration layers that integrate with EHRs, analytics, and CRM technologies.
- RPM alerts should update the EHR; physicians’ care notes should feed back into the RPM context.
Auditability, Compliance, and Trust
When CMS, payers, or internal quality teams need logs, can your RPM system deliver?
Key Compliance Considerations
- Time-stamped records for each alert, action, and escalation
- Who got the warning, and what actions were taken?
- Was the patient’s outcome documented?
Design Features that Enable Audit Readiness
- Built-in audit trail generators.
- Role-based access logs
- Integrated compliance dashboards.
These are used for more than simply audits; they also contribute to the system’s internal confidence.
Scaling Responsively: RPM Workflow Flexibility
Today’s RPM workflows may be effective for 100 patients, but what about 10,000 across chronic, acute, and preventive care? CTOs Should Plan for
- Configurable routing rules based on cohort or care pathway.
- Alert logic templates for several illness classifications.
- Automated load balancing for care teams during peak periods.
Related: How to Architect a Scalable RPM Platform for Multi-Condition Care Programs
Scale RPM Smarter with CapMinds
Monitoring data is only half the battle; turning it into timely, actionable care is where CapMinds excels.
Our end-to-end digital health services give CTOs the architecture, tooling, and 24/7 support needed to build RPM programs that scale without sacrificing signal quality.
- Interoperable RPM Platform: FHIR-first ingestion, device libraries, and cloud hosting
- Intelligent Data Routing: Condition-aware pipelines that prioritize critical vitals and trends
- Smart Clinical Alerts: AI-tuned thresholds, contextual messaging, and fatigue controls
- Escalation Workflows: Role-based ladders, time-bound triggers, and audit trails
- Analytics & Compliance: Real-time dashboards, CMS billing automation, HIPAA-ready logs
Whether you’re integrating 10 devices or 10,000, CapMinds designs repeatable frameworks that cut response time, safeguard revenue, and free clinicians to focus on care.
Book a strategy call today and see how quickly your RPM stack can move from data overload to decisive, life-saving insight.