Interoperability and Compliance: What It Takes to Pass CMS Audits
Data interoperability and regulatory compliance are complicated in the healthcare sector. The purpose of the CMS audits is to make sure that healthcare providers follow federal regulations on information security, clinical quality reporting, and patient data interchange. It takes careful design, strong interoperability frameworks, and proper documentation procedures to pass a CMS audit.
In this blog, you’ll learn the actual requirements for passing CMS audits from the point of interoperability and compliance.
The CMS Audit – Interoperability Is Now a Primary Priority
The scope of CMS audits has expanded beyond clinical documentation and billing accuracy. CMS is paying more attention to how well payers and providers can share health information thanks to rules like the Interoperability and Patient Access Final Rule.
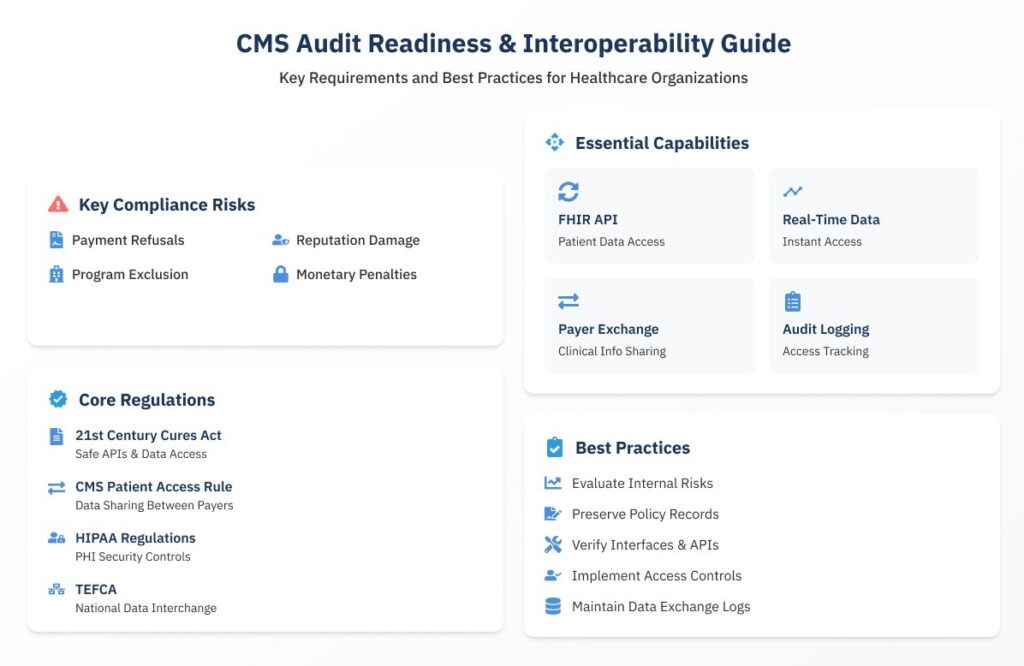
Interoperability is a compliance concern as well as a technological need. CMS interoperability requirements violations can lead to:
- Refusals or modifications of payments
- Damage to one’s reputation
- Absence of involvement in CMS initiatives such as Medicare Advantage
- Monetary civil penalties
Providers must show that their systems can safely and on-demand transmit PHI in light of CMS’s demands for increased transparency and data fluidity.
Key Regulations Driving CMS Audit Readiness
Preparing for CMS audits requires an understanding of the regulatory environment. The following mandates have a direct impact on audit criteria.
Act for 21st Century Cures
- Need safe APIs to provide patients with real-time access to data.
- Prohibits the blocking of information.
CMS Patient Access and Interoperability Rule
- Requires the sharing of data between payers.
- Requires the sharing of claims data and provider directories over FHIR-based APIs.
HIPAA Privacy and Security Regulations
- Control the safe sharing of PHI.
- Demand breach notification procedures, access limits, and audit trails.
Trusted Exchange Framework and Common Agreement
- Creates a platform for consistent data interchange across the country.
- It could soon be used as a standard for CMS interoperability evaluations.
Healthcare businesses must match these requirements with their compliance paperwork and data interchange capabilities in order to pass CMS audits.
Essential Interoperability Skills CMS Audited
CMS inspectors usually seek detailed proof that your health IT systems facilitate safe, consistent data sharing. Important interoperability features include:
- Enabling the FHIR AP – The ability to make patient data, such as clinical notes, prescriptions, allergies, and claims, available using HL7 FHIR APIs.
- Real-Time Data – Systems must provide prompt access to patient data, particularly for patient-generated health data and care transitions.
- Payer-to-Payer Exchange – Medicare Advantage plans need to show that they can share clinical information about patients with other payers when asked to do so.
- Logging Audits – Thorough audit trails that demonstrate who accessed what information, when, and why.
Best Practices for Compliance in CMS Audit Preparation
Being prepared for an audit begins long before CMS notifies you. Your chances of passing will be greatly increased if your company adopts compliance best practices.
1. Evaluate Internal Risks
- Assess data sharing procedures and security flaws regularly.
- Chart the data flow between various systems, such as patient portals, billing, and EHRs.
2. Preserve Records of Policies and Procedures
- Establish and revise SOPs for security, patient consent, and data exchange.
- Make sure employees are aware of the locations and methods for accessing policies.
3. Verify Your Interfaces and APIs
- API endpoints may be verified by using FHIR compliance testing tools.
- Make sure that there are no problems or timeouts when external apps access patient data.
4. Implement Robust Access Controls
- Regular credential audits, multi-factor authentication, and role-based access are crucial.
- CMS may conduct an audit on how you provide and remove system access.
5. Maintain Reports and Logs of Data Exchange
- Keep records of every data transfer, API request, and access event.
- During the audit, be prepared to export these logs in a format that can be read by humans.
Technical Infrastructure: Improving Interoperability and Compliance
CMS evaluates how your systems accomplish compliance, not simply the outcomes.
To create an audit-ready system, your architecture should include:
- The Unified API gateway simplifies data transmission across EHRs, laboratories, payers, and patient applications.
- FHIR server and data mapper convert old HL7 v2 or CDA data to FHIR-compliant formats for real-time access.
- Consent management engine captures, maintains, and applies patient consent choices to all outbound data transfers.
- Interoperability engines Mirth and InterSystems provide data transformation, routing, and validation between systems.
- The Compliance dashboard monitors API health, access activity, and audit logs from one single location.
This stack not only provides smoother operations, but it also accelerates and simplifies evidence collection for CMS audits.
Common Pitfalls That Cause Audit Failures
Even well-intentioned providers fall short of CMS audits owing to avoidable errors. Here are some of the frequent pitfalls:
- Outdated or Unsupported APIs – Using outdated formats rather than FHIR APIs, or failing to update endpoints regularly.
- Lack of Consent Tracking – Inadequate mechanism for capturing and implementing patient data sharing preferences.
- Inconsistent Data Mapping – Clinical data is not standardized, leading to missing or incorrect payloads.
- Inadequate Audit Trails – There are no verifiable logs of data access or disclosure, which breaches HIPAA and CMS guidelines.
- Poor Team Coordination – IT, compliance, and operations do not collaborate, resulting in policy and practice mismatches.
To avoid these challenges, you need a proactive compliance culture and a solid governance framework.
Role of Health IT Vendors and Consultants
Healthcare businesses are not required to manage interoperability compliance alone. Strategic partners can help you achieve and sustain audit preparedness.
- Implement and verify the FHIR APIs.
- Provide compliance audit templates and gap analysis.
- Provide centralized consent and access control systems.
- Monitor interface logs for real-time fault detection.
- Conduct simulated audits and employee preparedness training.
When selecting a partner, make sure they have previous expertise with CMS programs such as Medicare Advantage, QPP, and Medicaid Managed Care.
Related: How The CMS 2025 Interoperability Rule Transforms Healthcare Data Access And Compliance
Get CMS Audit-Ready With CapMinds Interoperability & Compliance Services
Passing CMS audits isn’t just about ticking checkboxes; it’s about proving your systems are secure, interoperable, and aligned with regulatory expectations.
At CapMinds, we simplify the complexity of interoperability and compliance with tailored digital health tech solutions that help you stay ahead of audits, penalties, and reputational risks.
Here’s how we support your audit readiness and long-term compliance:
- FHIR API Enablement for patient data access, payer exchange, and real-time insights
- Unified API Gateways to connect EHRs, labs, payers, and patient apps
- Custom Compliance Dashboards for real-time monitoring and audit log tracking
- Consent Management Engines that honor HIPAA and 42 CFR Part 2 rules
- Mirth & InterSystems Interface Development for seamless data transformation
- Gap Analysis & Simulated CMS Audit Programs to identify and fix weaknesses
Partner with CapMinds to build a compliant, connected, and audit-proof healthcare ecosystem.