Integrating Telehealth With EMRs, Labs, and Billing Systems: What Works
Telehealth usage has expanded dramatically, driven by patient demand and the need for flexible healthcare delivery. Many healthcare companies still struggle to efficiently integrate telehealth with EMRs, laboratories, and billing systems.
The seamless integration of these platforms provides efficient operations, accurate data flow, and improved patient experiences. In this blog, you’ll learn how to integrate telehealth with EMR, billing, and lab systems. Healthcare professionals should know how to ensure successful telehealth integration.
The Significance of Integration in Telehealth
- Holistic Patient View – To ensure continuity of treatment, clinicians using telehealth access the same patient history, prescriptions, and allergies that are kept in the EMR.
- Data Accuracy – By eliminating human entry mistakes, automated data flows guarantee that lab and billing records include the most recent clinical data.
- Operational Efficiency – Integrations simplify procedures for billing teams, lab technicians, and providers by removing double-entry.
- Patient Experience – Online appointments, lab orders, and invoicing are all streamlined for patients and handled behind the scenes.
Organizations may boost adoption, enhance results, and increase ROI by integrating telehealth with core healthcare systems.
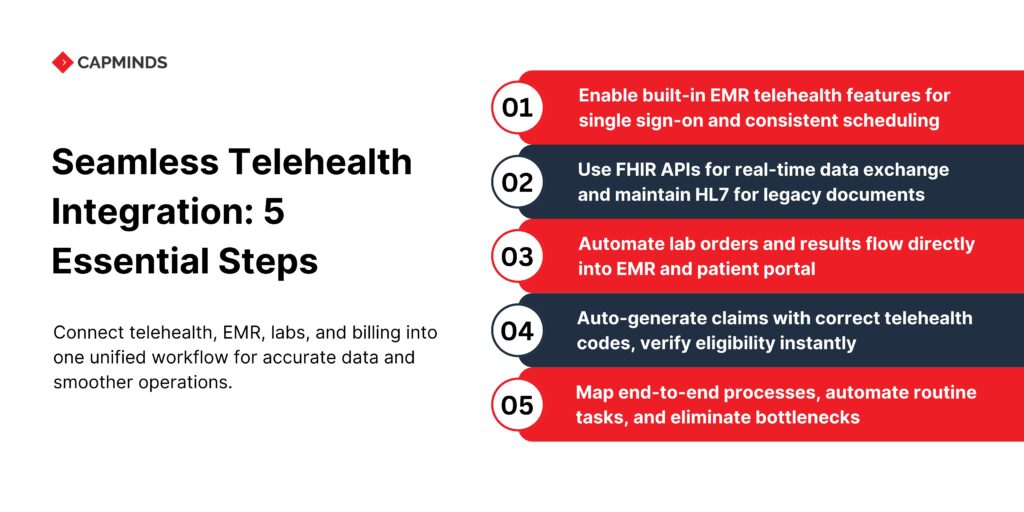
Best Practices for EMR–Telehealth Integration
1. Make Use of Local Telehealth Modules
- Numerous top EMR providers like Epic and Cerner provide pre-installed telehealth modules that need little setup.
- Single sign-on, uniform scheduling, and consistent branding are guaranteed via native modules.
2. Make Use of Standards-based APIs
- FHIR makes it easier to get encounter data, clinical notes, and patient details.
- CDA and HL7 communications are still dependable for document interchange in older systems.
3. Integrate Telehealth Connections into Workflow
- Incorporate “Start Telehealth Visit” buttons into appointment scheduling and patient records.
- Reduce context switching by allowing clinicians to initiate video conversations from within the EMR interface.
4. Align Documentation and Scheduling
- Create telehealth appointment times in the EMR calendar automatically.
- Directly enter visit notes, diagnoses, and follow-up orders from telehealth interactions into the patient’s chart.
5. Make Sure Data Flows Both Ways
- Update the EMR with encounter metadata start and finish timings, provider, and telehealth platform, followed by a telemedicine session.
- If required, push EMR updates back to the telehealth platform via webhooks or API callbacks.
Connecting Laboratory Systems to Telehealth
Remote lab ordering and result distribution are common components of a strong telehealth program. This is what functions:
1. Automated Lab Orders
- Lab orders should be triggered by doctors during the telehealth interaction and sent straight to the LIS.
- For order transmission, use FHIR’s ServiceRequest resource or HL7 ORM messages.
2. Visibility of Results in the Telehealth and EMR
- LIS should send FHIR DiagnosticReport documents or HL7 ORU messages to the EMR once labs are finished.
- The patient-facing dashboard of the telehealth portal allows patients to examine outcomes, encouraging patient participation.
3. Coordination of Specimen Collection
- Allow patients to schedule home specimen collections by integrating with phlebotomy or courier scheduling software.
- Using automated notifications, provide lab order information, collection guidelines, and courier tracking links.
4. Compliance and Quality
- Verify that lab integrations continue to adhere to HIPAA and CLIA regulations.
- Use TLS to encrypt HL7 channels and use audit logging for each message that is sent.
Seamless Integration of Billing Systems
1. Automate Claim Creation
- Use integrated practice management or RCM systems to automatically create electronic claims (837P/837I) following telehealth interactions that have been recorded in the EMR.
- Accurately map the CPT and HCPCS codes for telehealth (99441–99443, 99201–99215 with modifier 95).
2. Instantaneous Verification of Eligibility
- Use the clearinghouse API to verify the patient’s insurance eligibility and telehealth coverage before or during scheduling.
- Show coverage information on the portal to patients or scheduling staff.
3. Monitor Telehealth-Specific Guidelines
- Include payer-specific guidelines in the billing engine, such as requirements for the originating site and restrictions about technological fees.
- Add necessary modifiers, such as GT, 95, and place-of-service codes like POS 02, automatically.
4. Denial Management and Dunning
- Set up the billing system to quickly follow up on telehealth claims that have been refused or are pending.
- To help teams address the underlying problems, provide dashboards that display refusal reasons, including code, eligibility, and documentation.
5. Patient Payments and Statements
- Create patient statements that include facility, professional, and technology fees for telehealth appointments.
- Connect to patient payment portals to enable automatic payment plans and online bill payment.
Optimizing Virtual Care Workflows
Workflows for virtual care that are effective mostly depend on integrated technology systems. Doctors may streamline patient interactions from scheduling appointments to following up after visits by integrating telehealth solutions with EMRs, labs, and billing systems.
Successful workflow optimization requires telehealth processes to be clearly described, bottlenecks to be identified, and routine operations to be automated using integrated technology.
To improve overall operational efficiency, providers should deploy linked care systems that allow for customized workflows, flexible scheduling, and proactive patient interaction.
Key Points for Workflow Optimization
- Clear process mapping
- Automation of everyday chores
- Flexible, patient-centered scheduling
Choosing Connected Care Platforms
For telehealth integration to be successful, choosing the right connected care platform is essential. Platforms with robust integration capabilities, intuitive user interfaces, and secure, legal data management should be prioritized by providers. Payment integration, lab data communication, and EMR interoperability are all facilitated by dependable connected care systems.
Before picking a platform, providers should consider its capacity to expand with growth, integrate with current systems, and ensure consistent performance.
Comprehensive support and maintenance services guarantee that the platform can handle changing clinical and operational needs successfully.
Key Factors for Selecting Linked Care Platforms
- Strong integration capability
- Scalability and Reliability
- Comprehensive support and maintenance services
Best Practices for Effective Telehealth Integration
Healthcare institutions can employ a few recommended practices to guarantee effective integration:
- Conduct rigorous needs assessments to clearly define integration requirements.
- Engage physicians and administrative personnel early in the planning and implementation phase.
- Establish explicit integration goals and performance indicators to track progress.
- Provide continual staff training and education about integrated telehealth systems.
- To meet evolving healthcare demands, examine and upgrade integration procedures and technology regularly.
Related: Using OpenEMR as the Core for Your Digital Health Platform (RPM, Telehealth, Labs, AI)
Enhance Your Telehealth Integration with CapMinds Digital Health Solutions
CapMinds Services delivers comprehensive digital health tech solutions tailored to optimize your telehealth ecosystem.
Whether integrating telehealth with EMRs, streamlining lab data exchange, or improving telehealth billing systems, our advanced solutions simplify complex workflows and drive operational efficiency.
- Telehealth & EMR Integration: Seamlessly connect telehealth platforms with EMRs for real-time patient data synchronization.
- Lab Data Exchange Solutions: Ensure secure and timely integration of lab results using standard protocols (HL7, FHIR).
- Efficient Billing Integration: Accelerate your reimbursement processes and eliminate billing complexities through automated telehealth billing integration.
- Customized Virtual Care Workflows: Design flexible, patient-centered workflows to boost clinical productivity.
- Connected Care Platforms: Robust, scalable telehealth platforms supported by comprehensive maintenance and real-time monitoring.
Partner with CapMinds to elevate your telehealth services, enhance patient outcomes, and secure sustainable growth for your healthcare organization.