Cost of Ignoring Legacy Infrastructure Risks in Healthcare
Digital technologies are essential to many aspects of modern healthcare, including scheduling, imaging, invoicing, and decision support. But a large number of American hospitals and health systems continue to use software that was created many years ago. Legacy databases, mainframe EMRs, and billing programs may still run core applications because they “work for now.” They also hide systemic risks.
Outdated software isn’t merely inconvenient; it is a threat to patient safety, regulatory compliance, and the bottom line. This post unpacks why ignoring aging infrastructure in healthcare is no longer an option and outlines a path toward safer modernization.
Legacy Infrastructure in Healthcare Is Widespread
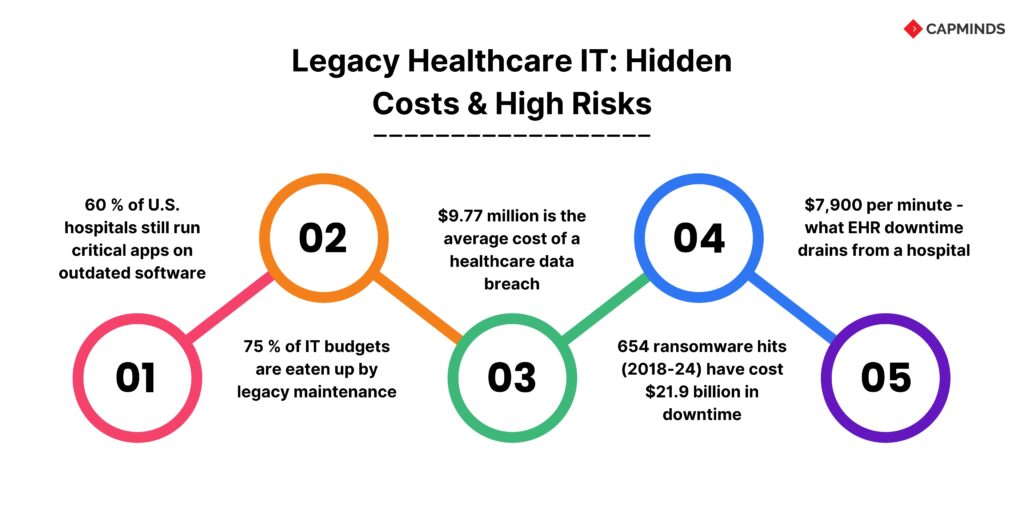
Legacy infrastructure in healthcare is deeply rooted. More than 60% of hospitals in the United States continue to employ at least one vital application that is dependent on old software. This program does not have FHIR-based interoperability, modern APIs, or cloud readiness. Hospitals typically run 200–300 distinct systems, many of which are incompatible with one another. This leads to data gaps that complicate the integration of telehealth, AI, and analytics and interfere with coordinated treatment. When an aged system malfunctions, it can endanger lives and is no longer merely a small frustration.
A 2025 case described by Futura Works shows what happens when a health system’s EHR crashes: physicians lost access to critical patient histories for hours, medication orders were delayed, and staff were forced to write on paper. The culprit was a 15‑year‑old system that had been flagged for replacement multiple times.
Old Systems Consume Budgets
Keeping outdated systems running isn’t cheap. Maintaining legacy platforms consumes up to 75 % of IT budgets. This restricts the innovation potential. Hospitals that use old platforms invest money in specialized personnel, hardware updates, and fixes. It would be more beneficial to use these resources to create new capabilities.
Within three years, phased modernization can cut IT operating expenses by 25–40%, starting with high-risk backend systems. Modernization not only lowers maintenance costs but also frees funds for strategic initiatives such as artificial intelligence and population health tools.
The need is urgent: healthcare IT spending on AI is expected to grow 40 % by 2026, yet many hospitals can’t deploy AI effectively because legacy systems can’t support it.
Security Vulnerabilities and Breach Costs
Security is the most visible risk. Healthcare has topped IBM’s “Cost of a Data Breach” industry ranking for years. In 2023, the average healthcare data breach cost $10.93 million.
- The number has fallen to $9.77 million, yet healthcare remains the costliest industry for breaches.
- Even a small reduction doesn’t change the fact that a single incident can wipe out millions in revenue and trust.
- 83 % of healthcare organizations experienced a breach in the past two years.
- Attackers target hospitals because legacy systems often run unpatched software and outdated encryption.
More than half of hacking‑related breaches focus on network servers, many of which run out‑of‑support operating systems. That means an attacker only needs to find an old server or a device running Windows XP to gain access to patient records.
Ransomware and Downtime
Ransomware makes these vulnerabilities tangible.
- 654 ransomware incidents targeting U.S. healthcare organizations between 2018 and 2024.
- Those attacks compromised nearly 89 million patient records and produced $21.9 billion in downtime costs.
- The financial impact of downtime averaged $1.9 million per day per organization, and recovery periods lasted over 17 days on average.
- Individual cases illustrate how severe these events are.
- Ascension’s 2024 ransomware attack disrupted 140 hospitals and is expected to cost $1.1–1.6 billion in recovery and lost operations.
- A similar attack on CommonSpirit Health in 2022 cost $160 million, while Scripps Health lost $112.7 million after a 2021 breach.
These figures show that delaying modernization isn’t about saving money; it’s about gambling with budgets and reputations.
The Hidden Cost of Downtime
Aging infrastructure is not only susceptible to ransomware. Routine downtime for EHRs and lab systems incurs huge costs. Hospitals pay an average of $7,900 per minute of EHR downtime.
Due to postponed treatments and cancelled appointments, a single interruption can cost over $208,600 in direct income. Healthcare institutions may have to pay up to $1.19 million every day for downtime. More than 17 days may pass before the problem is completely fixed.
Clinicians frequently resort to manual procedures and paper charts during an outage. This raises the possibility of mistakes and delays in care. Unexpected interruptions caused a 62% delay in lab results. Patient outcomes may be impacted by these delays. Critical lab work may be sent to outside institutions, surgeries may be delayed, and emergency cases may be diverted to nearby hospitals.
Some hospitals spend more time on manual workarounds than on patient care, and every minute of disruption exacerbates waste and frustration. Clinicians already spend up to 45 % of their day on administrative or non‑clinical tasks due to outdated user interfaces. Downtime only increases that burden.
Compliance and Regulatory Pressure
Healthcare IT modernization isn’t just a best practice; it’s becoming a regulatory mandate. The 21st Century Cures Act and the Trusted Exchange Framework and Common Agreement require real‑time data exchange and interoperability.
AI-driven efficiencies and better patient access are being promoted by the Office of the National Coordinator for Health IT and the Centers for Medicare & Medicaid Services.
Meanwhile, modifications to HIPAA’s Security Rule is anticipated in 2025. Stronger defenses against vulnerabilities in legacy systems will be necessary for this update. Hospitals that continue to use antiquated procedures run the danger of non-compliance and penalties. Modernization is now necessary to meet changing security and interoperability standards; it is no longer optional.
Operational Inefficiencies and Poor Interoperability
Not only does legacy infrastructure affect security and compliance, but it also reduces productivity. Numerous stand-alone systems are used in hospitals. Clinicians have to manually merge data and handle several logins. Incompatible interfaces slow down workflows and cause duplication of data.
Infusion pumps for medical use and nurse-call systems are only two examples of the many mission-critical equipment that continue to operate on unsupported operating systems. Software on one out of every five linked medical equipment is out of security upgrades.
Staff members use spreadsheets and paper charts as workarounds when systems are unable to communicate. Errors are introduced by these manual procedures. They can make it challenging to coordinate care across departments or spot trends.
These workarounds put new digital ventures at a disadvantage. Clean, connected data streams, not disjointed gaps, are necessary for telehealth platforms and AI-powered diagnoses.
High Maintenance Costs and Workforce Challenges
Keeping legacy systems alive demands specialized expertise. Many older platforms were built in languages that run on hardware that is no longer supported. Finding staff who can maintain them is increasingly difficult. Knowledge of older systems is lost when seasoned employees retire.
Hospital budgets are also under strain from declining reimbursements and growing labor costs. Modernization may seem expensive to executives. But the hidden costs of legacy systems, such as reactive break-fix work, lengthy maintenance periods, and training on antiquated technology, mount up quickly.
Clinical operations are still disrupted, for example, when a hospital plans frequent outages to patch old servers. Unexpected outages might cause as much disruption as regular maintenance windows. They restrict capacity and disrupt workflows.
The Financial Case for Modernization
While replacing legacy systems requires investment, the return on modernization is clear.
Hospitals adopting modular, phased modernization see operational cost reductions of 25–40 % within three years. Modern architectures use cloud services, APIs, and microservices to decouple old systems without a full rip‑and‑replace.
- They also enable resilience and scalability, two crucial factors as patient volumes grow.
- The global healthcare IT market is expected to reach $354.04 billion in 2025 and could grow to $981.23 billion by 2032, reflecting a 15.7 % compound annual growth rate.
- A significant portion of that spend, up to 60–70 %, is currently dedicated to modernizing existing systems.
- Those numbers underline how industry leaders are prioritizing infrastructure upgrades.
- The remaining 30–40 % of budgets fund new technologies such as AI diagnostics and telehealth platforms.
The choice is between funneling resources into patching outdated systems or investing in solutions that improve patient outcomes and reduce long‑term risk.
Case for Risk Reduction
Modernization reduces not only operating costs but also the magnitude of risk. Hospitals with security AI and automation reduce breach costs by an average of $2.2 million.
By adopting zero‑trust architectures, encryption at rest and in transit, and real‑time monitoring, organizations can shorten the time to detect and contain threats.
- The 2024 IBM report found that the average time to identify and contain a breach dropped to 258 days, the lowest in seven years, but it still underscores how slowly defenders react.
- Shorter breach lifecycles translate to lower costs; breaches resolved within 200 days are substantially less expensive.
- Modern analytics and automation accelerate detection and response, helping hospitals avoid the worst outcomes.
A Roadmap to Modernization
Modernizing old infrastructure is not an easy task. A gradual, risk-based approach is frequently the most successful. Healthcare IT leaders can use a systematic roadmap:
Assessment and prioritizing.
- Audit all systems, dependencies, and data gaps.
- Determine the security vulnerabilities, compliance gaps, and clinical relevance of each system.
- Prioritize updates according to risk exposure and patient impact.
Strategy Selection
- Choose whether to rehost, replatform, restructure, or replace each system.
- Align the plan with regulatory deadlines and patient-experience objectives.
Architectural design.
- Implement a modular, API-first architecture.
- Use cloud services such as AWS HealthLake or Azure Health Data Services to provide real-time data transmission with HL7 FHIR.
- Interoperability layers eliminate vendor lock-in while improving data flow.
Data Migration and Security
- Clean up and validate legacy data.
- Encrypt it both during transit and at rest.
- Create role-based access controls, audit trails, and incident response methods.
Clinical engagement and change management
- Co-design workflows with end users to guarantee that new systems can support daily tasks.
- Implement changes in phases, provide training, and track feedback.
Pilot projects and iterative deployment
- Begin with low-risk departments, assess results, and scale based on lessons gained.
- Continuous improvement ensures that technological investments remain aligned with clinical needs.
Hospitals that follow this approach can reduce interruptions and immediately experience advantages. Modernization is more than just installing new software; it is also a cultural shift toward data-driven care and continual improvement.
Related: Cut EHR Licensing Costs by 60%: OpenEMR vs. Legacy Systems for Enterprise-Scale Operations
Accelerate Your Healthcare IT Modernization
Don’t let legacy infrastructure jeopardize your hospital or clinic’s future.
At CapMinds, we offer comprehensive digital health tech services that guide you through a smooth and efficient transition to modern, scalable systems.
Our team is dedicated to helping healthcare organizations like yours reduce operational inefficiencies, mitigate risks, and ensure compliance with the latest regulations. Our Services
- Telehealth Platform Development – Seamlessly integrate virtual care with patient-centric services.
- Custom Software Development – Tailored solutions to meet your unique operational needs.
- Health IT Modernization – Upgrade outdated systems for enhanced performance, security, and compliance.
- Interoperability Solutions – Achieve seamless data exchange across all systems.
- Cybersecurity – Protect patient data with robust, next-gen security protocols.
Why Choose CapMinds:
- Proven Expertise: A track record of successful healthcare IT projects.
- Cost-Effective Solutions: Save on maintenance and downtime costs.
- Customizable Services: Designed to meet your clinic’s specific needs.
Let us help you modernize your healthcare infrastructure to improve patient care and operational efficiency. Contact us to start your Healthcare IT Modernization transformation.