How Modular Architecture Saves Millions in Digital Health Infrastructure Over the Long Run
Health systems and hospitals today confront two challenges. Demands from rapidly evolving technology and ongoing cost-cutting pressures. Attempting to handle everything at once, traditional all-in-one healthcare IT solutions can become rigid and costly to operate. In a monolithic system, any new feature or integration may need extensive platform-wide testing and redesign, increasing expenses and delaying advancement. A better long-term approach is modular architecture, which designs IT systems as a collection of separate, compatible modules.
By moving away from rigid monolithic solutions, a modular approach offers improved flexibility, scalability, and cost-efficiency, key advantages in today’s fast-evolving healthcare landscape.
Over time, this translates into substantial savings, potentially saving millions in infrastructure and operational costs as the system grows and adapts.
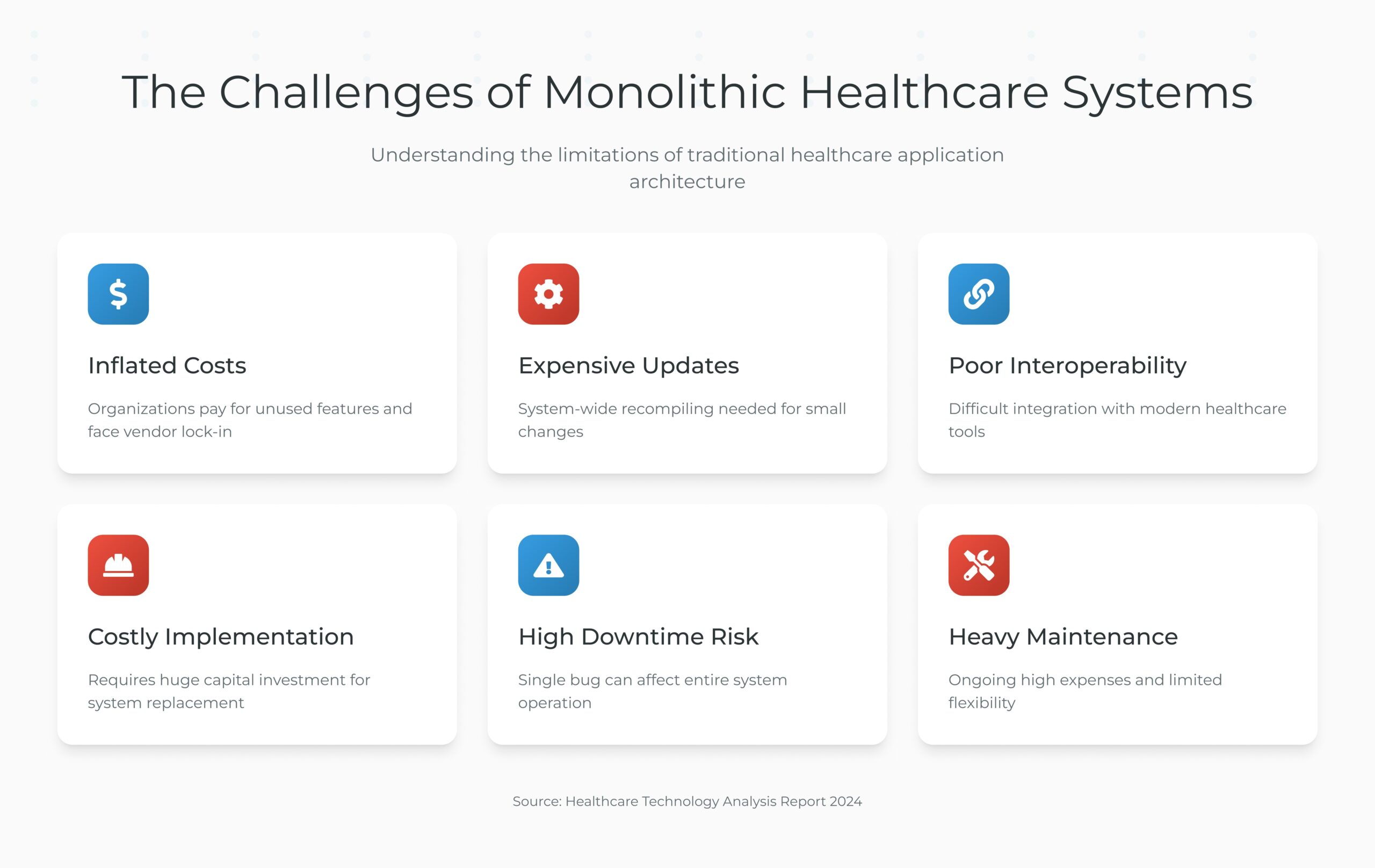
The High Cost of Monolithic Healthcare Systems
Monolithic healthcare applications (like legacy electronic health records or hospital information systems) combine all features into a single, tightly integrated solution. This can result in expensive costs and create vendor lock-in; essentially organizations are paying for features they may not be using and becoming dependent on the vendor’s ecosystem. Further, version upgrades or customizations to monolithic systems tend to be costly.
One example is that making a small change in one component can mean recompiling and retesting the entire monolithic system. Updating monolithic systems takes a lot of time which leads to lengthy development cycles and higher labor costs.
- Legacy monolithic systems frequently lack easy integration points, making interoperability with new tools difficult.
- Hospitals find themselves either stuck with outdated capabilities or forced into “big bang” replacements that require huge capital investments to implement a brand new system all at once.
- Moreover, monoliths carry a higher risk of downtime.
- A single bug or failure can bring down the whole application, potentially interrupting care and incurring revenue losses.
- The traditional one-size-fits-all architecture often becomes a nightmare of high maintenance expenses, costly upgrades, and limited agility.
What Is Modular Architecture in Digital Health?
Modular architecture is designated “modular” because the entire architecture is divided into discrete components that are autonomous but interdependent. The modules can be developed, updated, and scaled independently.
Every module will carry out a specific task, such as telemedicine, electronic health records, invoicing, appointment scheduling, patient registration, etc.
- These components are made to communicate with one another using APIs, or well-defined interfaces, rather than a close coupling of code.
- This makes it possible to replace or modify a single module or component without having to rebuild or modify the components on either side.
- Healthcare IT teams have the freedom and agility to build new features or upgrades of the application in phases, one module at a time, when applications are designed as a collection of interchangeable apps.
- To make sure that components may share and use common interoperable capabilities despite being loosely connected, the modular, or loosely coupled, architecture might be made up of plug-ins, micro services, or open standards.
- Compared to a monolithic program, this results in a system architecture that is significantly more adaptable and scalable and that is much simpler to adapt and alter at a lower cost and effort.
How Modular Architecture Cuts Costs in the Long Run (Key Benefits)
Adopting a modular architecture isn’t just a technical decision. It’s a strategic investment that pays off in reduced total cost of ownership over the long run. Below are several key ways that modular design in digital health infrastructure leads to significant cost savings:
1. Incremental Scalability and “Pay-as-You-Grow”
Modular design allows health IT systems to scale gradually, adding new modules or capacity only as needed instead of committing to expensive full-system upgrades upfront.
- For example, if a hospital needs to expand telehealth services, it can deploy a telehealth module and integrate it with the existing system, rather than purchasing a whole new monolithic system.
- This targeted scaling means you invest in additional infrastructure or licenses only for the areas of growth, avoiding waste.
- Choosing a modular architecture lets your system grow with your practice.
- It’s far cheaper to scale an efficient base than to rebuild from scratch when new needs emerge.
- You can align IT spending with actual needs over time, preventing over-provisioning and large sunk costs.
2. Faster Development and Reduced Upfront Costs
Module-based software allows teams to develop and deliver components independently, enabling teams to stay productive while working on the related components in parallel on different schedules. If there are 4 components in the system, with 1 of those being ‘the system’, the development of each component doesn’t need to be done sequentially. There is no need to stop the entire system for every change.
Updates, new functionality, or other improvements can all be released in one module, while still ensuring that other modules are not broken.
This concurrent development and deployment increases time-to-market and lowers costs by eliminating the expensive system-wide testing that comes with the monolithic updates.
Reusability is promoted by modular architecture, which allows common functionality to be created once as modules and utilized by several departments or applications. Over time, cost reductions result from the elimination of duplicate development work caused by reusing existing modules for new projects.
Related: EHR in 90 Days: Accelerating Digital Transformation in Healthcare
3. Reduced Downtime and Simplified Maintenance
Maintaining a modular system is simpler and less costly. Since each module can be tested and debugged separately rather than needing to search through a huge codebase, it is simpler to isolate errors in a modular network.
A bug in one module is less likely to impact the other parts of the system, as that would limit the scope of the bug and ideally, it would allow that issue to be solved faster with minimum disruption. No need to take the system completely down for a bug in one module, you can make a change to a single module without outages or downtime for the full repair. Updates or patches can be done to a single module, constrained on the module with minimal impact or downtime in maintenance windows.
All of this leads to lower support and maintenance costs: IT staff can focus on the specific modules that need work, and fewer emergency “all-hands” situations arise from system-wide failures.
A modular system will be cheaper to maintain as the environment changes since you will only need to upgrade or replace some old modules, rather than rebuilding the entire system. Expansion will be less costly to adapt since the overall system has considerably more life and less daunting financial commitment than having to entirely replace a legacy system all at once.
4. Eliminating Redundancies and Separated Systems
Large healthcare enterprises often end up with siloed systems. This duplication drives up infrastructure and licensing costs, as you’re paying multiple times for similar capabilities. Modular architecture enables the consolidation of common functions into shared services, cutting out redundant systems.
Rather than each specialty department maintaining separate data silos or imaging archives, a modular approach can centralize those in one repository that all relevant modules use.
- A real-world example is the trend toward vendor-neutral archives in medical imaging.
- Rather than every department managing an individual Picture Archiving and Communication System, the hospitals use one central VNA module for storage, and individual viewer modules connect to it.
- This eliminates duplicate storage, servers, and ongoing support contracts, which allows hospitals to save tremendously over time and in fixed costs relative to infrastructure, licensing, and maintenance operational overhead.
- A modular approach fosters effectiveness by leveraging common resources across the organization and together using less IT footprint, serving several functional needs.
5. Freedom from Vendor Lock-In
Modular systems are usually based on clear interfaces and open standards, and healthcare organizations have greater freedom to select or switch providers for individual components. Not every component of your system must be purchased from a single mega-vendor.
- This prevents the high-cost trap of vendor lock-in, where proprietary monoliths force you to pay whatever the vendor demands for expansions or upgrades.
- With a modular platform, you have the freedom to choose the best-of-breed solution for each functionality without being locked into one company’s ecosystem.
You might use one vendor’s EHR module, but if their telehealth module is too pricey or subpar, you can integrate a different telehealth product into your architecture.
- Data and logic aren’t tied up in one proprietary system, so if you don’t like a module, you can replace it without overhauling everything.
- This competitive flexibility often leads to better pricing and innovation from vendors, ultimately saving costs.
- Avoiding vendor lock-in means you only pay for what you truly need.
- As a LinkedIn analysis pointed out, bundled monolithic systems often force buyers to pay for unnecessary features, inflating costs.
- Modular design lets you break that bundle apart.
6. Future-Proofing and Innovation Agility
Healthcare technology is changing quickly. A modular architecture that allows hospitals and health systems to quickly and easily adjust their model of care without large capital purchases is constantly being improved, added to, and integrated. Innovations or technologies can be added as new module or components that stand alone as both hard and soft technologies, but operate in conjunction with a larger operational technological platform.
If a hospital or plan wants to apply machine learning to predictive analytics, it can simply attach an AI module to the platform and load it with the data through appropriate APIs. Modular platforms allow organizations to adopt innovations like AI applications without the expense and headache of modifying or building a new complete system. The same is true for regulatory or other new compliance requirements.
- We can make updates to an affected module without needing to rewrite the whole application.
- This speed and flexibility to pivot based on external changes helps you to keep your system relevant and mitigates against being stuck with obsolete technology.
- This does give you confidence that a well-designed modular system is future-proof and will quite literally save you millions by avoiding a rip-and-replace of your digital health platform every time there is a technology upgrade or a policy change.
- Over the long run, this provides sustainable cost savings by extending the life and usefulness of your investments.
Future-Proof Your Health System with CapMinds Modular Digital Health Solutions
At CapMinds, we help healthcare organizations eliminate the cost burdens of rigid, outdated systems through future-ready modular solutions.
Our digital health tech services are designed to integrate seamlessly, evolve independently, and scale as you grow, saving you millions in infrastructure and operational costs.
Whether you’re transitioning from monolithic platforms or building a modern health IT stack from the ground up, we’ve got you covered with:
- Custom Healthcare Software Development
- Modular EHR Services & Solutions
- Healthcare Interoperability Platforms (HL7, FHIR, API)
- Telehealth & Remote Patient Monitoring Modules
- Medical Billing & Revenue Cycle Management Tools
- Hospital Inventory & Procurement Systems
- Data Warehousing & Advanced Analytics Dashboards
- CRM Systems Tailored for Healthcare Workflows
Break free from vendor lock-in, reduce unnecessary spend, and unlock long-term value with modular digital infrastructure.
Let CapMinds help you modernize your digital health strategy.